 |
| Different Components of Blood |
Blood:
Blood is a connective tissue. It provides one of the means of communication between the cells of different parts f the body and the external environment, e.g. it carries:
1) Oxygen from lung to tissues and carbon-Di Oxide from the tissue to the lung for excretion.
2) Nutrients from the alimentary tract to the tissues, and cell wastes to the excretory organs. Principally the Kidneys.
3) Hormone secreted by the endocrine glands to their target glands and tissues.
4) Protective substance, e.g. antibodies, to areas of infection.
5) Clotting factors that coagulate blood, minimising bleeding from ruptured blood vessels.
Blood makes up 7% of the body weight.
ERYTHROCYTES (RED BLOOD CELLS):
This cells are biconcave disks; they have no nucleus, and their diameter is about 7 micrometres.Their main function is in gas transport, a mainly of oxygen, but they also carry some carbon dioxide.Their characteristic shape is suited to their purpose; The biconcavity increases their surface area for gas exchange, and the thinnest of the central portion allows fast entry and exit of gases.The cells are flexible so they can squeeze through narrow capillaries, and contain no intracellular organelles, leaving more room for haemoglobin, the large pigmented protein responsible for gas transport.Measurements of red cell numbers, volume and haemoglobin content are routine and useful assessments made in clinical practice.
 |
| Red Blood With Plasma |
PLASMA:
Blood consist of transparent fluid (Plasma) and blood cell. Plasma constitutes about 55% adn cell about 45% of blood volume. This constituents of plasma are water (90 to 92%) and dissolved substances, including:
Plasma Proteins
Inorganic Salts
Nutrients,principally from digested foods
Waste materials
Hormones
Gases.
Plasma proteins:
Which make up about 7% of plasma, are normally retained within the blood, because they are too big to escape through the capillary pores into the tissues.They are largely responsible of creating osmotic the pressure of blood ,which keep plasma fluid within the circulation.If plasma protein levels fall,because either reduced production or loss from the blood vessels, osmotic pressure is also reduced, and fluid moves into the tissue and body cavities.
Albumins: These are formed in the liver.They are the most abundant plasma proteins and their main function
is to maintain normal plasma osmotic pressure.Albumin also act as carrier molecules for
lipids
and steroid hormone.
Globulins: Most are formed in the liver and the remainder in lymphoid tissue.Their main functions are:
as antibodies (immunoglobulins). Transportation of some hormones and mineral salts.
Clotting factors: Fibrinogen is synthesised in the liver and is essential fro blood coagulation.
PLATELETS (THROMBOCYTES):
These are very small non-nucleated discs, 2 to 4 um in diameter, derived from the cytoplasm of megakaryocytes in red bone marrow. They contain a variety of substances that promote blood clotting, which causes haemostasis (cessation of bleeding).
The normal blood platelet count is between 200 * 10|9/1. The control of platelet production is not yet entirely clear but one stimulus is a fall in platelet count. The kidneys release a substances called thrombopoietin. Which stimulates platelet synthesis; other cytokines may also be involved.
The lifespan of platelets is between 8 and 11 days and those not used in haemostasis are destroyed by macrophages, mainly in the spleen.
Haemostasis:
When a blood vessel is damaged, loss of blood is stopped and healing occurs in a series of overlapping processes, in which platelets play a vital part.
Vasoconstriction: When platelets come into contact with a damaged blood vessel, their surface becomes stick and they adhere to the damaged wall. Then they release serotonin, which
consticts (narrows) the vessel, reducing blood flow through it.
Platelets plug formation: The adherent platelets clump to each other and release, other substances, including
ADP which attract more platelets to the site.Passing platelets stick to those already at the damaged vessel and they too release their chemicals.
 |
| Blood Clotting Process |
Coagulation (blood clotting): This is a complex process that also involves a positive feedback system and only a
few stages are included here
I Fibrinogen
II Prothrombin
III Thromboplastin
IV Calcium
V Proaccelerin, Ac-globulin
VII Proconvertin
VIII Antihaemophilic globulin (AHG)
IX Christmas factor, (PTA)
X Stuart Power Factor
XI Plasma thromboplastin antecedent (PTA)
XII Hageman factor
XIII Fibrin stabilising factor
Vitamin K is essential for synthesis of factors II,VII,IX and X.
 |
| Percentage of Different Components in Blood. |
LYMPHOCYTES (AGRANULOCYTES):
Lymphocytes are smaller than monocytes and have large nuclei. They circulate in the blood and are present in great numbers in lymphatic tissue such as lymph nodes and the spleen. Lymphocytes develop from pluripotent stem cells in red bone marrow and from precursors in lymphoid tissue elsewhere in the body where they are activated, i.e, they become immunocompetent which means they are able to respond to antigens example of antigens include: Cells regarded by lymphocytes as abnormal, e.g. cells that have been invaded by viruses,cancer cells,tissue transplant cells.
Pollen from flower and plants.
Fungi
Bacteria
Some large molecule drugs, e.g. Penicillin, Aspirin.
Although all lymphocytes originate from one type of stem cell, when they are activated in lymphatic tissue, two distinct types of lymphocyte are produced T-Lymphocytes and B-Lymphocytes.
B-LYMPHOCYTES:
These are both produced and processed in the bone marrow. Their role is in production of antibodies (immunoglobulins),Which are proteins designed to bind to and destroy, an antigen.As with T-lymphocytes, each B-lymphocyte targets one specific antigen; the antibody released reacts with one type of antigen and no other. B-lymphocytes provide antibody mediated immunity .
From this description of T-lymphocyte and B-lymphocytes, it is clear that for every one of the millions of possibleantigens that might be encountered in life there is one corrosponding T-Lymphocyte and B-Lypmphocyte. There is therefore a vast number of different T and B -lymphocytes in the body each capable of responding to only one antigen.
 |
| Different B and T cells |
T-LYMPHOCYTES:
These are processed by the thymus gland, which lies between heart and the sternum.The hormone thymosin, produced by the thymus, is responsible for promoting the processing, which leads to the formation of fully specialised, mature,functional
T-lymphocytes.It is important to recognise that a mature T-Lymphocyte has been programmed to recognise only one type of antigen, and during its subsequent travels through the body will react to no other antigen however dangerous it might be. Thus a T-lymphocyte manufactured to recognise the chickenpox virus will not react to a measles virus, a cancer cell, or a tuberculosis bacterium.T-lymphocytes provide cell-mediated immunity.
BASOPHILS (LEUKOCYTES):
Basophils, which are closely associated with allergic reactions, contain cytoplasmic granules packed with heparin(an anticoagulant), histamin (an inflammatory agent) and other substances that promote inflammation. Usually the stimulus that causes basophils to release the contents of their granules is an allergen (an antigen that causes allergy)of some type.This binds to antibody-type receptors on the basophil membrane.A cell type very similar to basophils, except that it is found in the tissues, not in the circulation, is the mast cell .Mast cells release their granule contents within seconds of binding in allergen, which account for the rapid onset of allergic symptoms following exposure to, for example,pollen in hay fever .
 |
| Different Components of Blood |
EOSINOPHILS (LEUKOCYTES):
Eosinophils , although capable of phagocytosis, are less active in this than neutrophils; their specialised role appears to be in the elimination of parasites, such as worms which are to big for phagocytosed.They are equipped with certain toxic chemicals, stored in their granules, which they release when the eosinophils binds an infecting organism.
NEUTROPHILS (LEUKOCYTES):
Their main function is to protect aganist any foreign material entering the body, mainly microbes,and to remove waste materials, e.g. cell debris.They are attracted in large numbers to any area of infection by chemical substances,released by damaged cells called chemotaxins. Neutrophils are highly mobile, and squeeze through the capillary walls in the affected area by diapedesis . Thereafter they engulf and kill the microbes by phagocytosis. Their nuclei are characteristically complex, with up to 6 lobes, and their granules are lysosomes containing enzymes to digest engulfed material.Pus that may form in an infected area consists of dead tissue cells,dead and live microbes and phagocytes killed by microbes. Their number are increased in:
Microbial infection.
Extensive tissue damage, miocardial infraction, burns, crush injuries.
Metabolic disorders, e.g. acute gout.
Leukamia.
Heavy smoking.
Use of oral contraceptive.
 |
| Human Blood Groups in 3D tabular form |
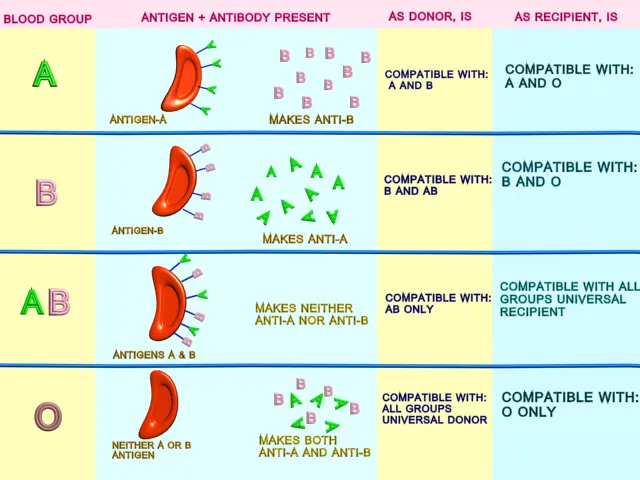
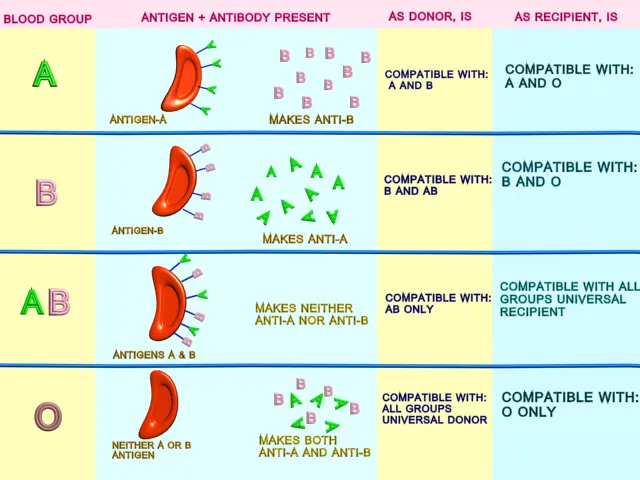
THE ABO SYSTEM:
About 55% of the population has either A-type antigens (blood group A) , B-type antigens (blood group B) or both (blood group AB) on their red cell surface.The remaining 45% have neither A nor B type antigens (blood group O). The corresponding antibodies are called anti-A and anti-B.Bllod group A individuals cannot make anti-A (and therefore do not have these antibodies in their plasma).Since otherwise a reaction to their own cells would occur.Since otherwise a reaction to their own cells would occur. They do , however, make anti-B.Blood group B individuals for the same reason make only anti-A.Blood group AB make neither,and blood group O make both anti-A and anti-B.
Because blood group AB people make neither anti-A nor anti-B antibodies, they are known as universal recipient: Transfusion of either type A or type-B into these individuals is likely to be safe,since there are no antibodies to react with them.Conversely, group O people have neither A nor B antigens on their red cell membranes, and their blood may.safely transfused into A, B, AB, O types: group O is known as universal donor. The terms universal recipient: and universal donor are misleading, however since they imply that the ABO system is the only one that needs to be considered. In practice although the ABO systems may be compatible, other antigen system on donor/recipient cells may be incompatible, and cause a transfusion reaction.For this reason prior to transfusion, cross matching is still required to ensure that there is no reaction between donor and recipient bloods.
Haemoglobin:
 |
| 3D Picture of Haemoglobin |
This is large, complex protein containing a globular protein (Globin)and a pigmented iron containing complex called Haem. Each haemoglobin molecule contains 4 Globin chains and 4 haem units each with one atom of iron. As each atom of iron can combine with oxygen molecule, this means that a single haemoglobin molecule can carry upto 4 molecule. An average red blood cell carries about 280 million haemoglobin molecules, giving each cell a theoritical oxygen carrying capacity f Over a billion oxygen molecules.
Haemoglobin + Oxygen <======> Oxyhaemoglobin
(Hb) (O2) (HbO)
Blood rich in oxygen is bright red because f the high levels of (HbO) it contains, compared with blood with lower oxygen levels which is dark bluish in colour because it is not saturated.
IMMUNOLOGICAL SURVEILLANCE:
A population of lymphocytes, called natural killer (NK) cells, constantly patrol the body searching for abnormal cells. Cells that have been infected with a virus, or mutated cells that have been infected with a virus, or mutated cells that might become malignant, frequently display unusual markers on their cell membranes, which are recognised by NK cells.Having detected abnormal cell, the NK cell immediately kills it. Although NK cells are lymphocytes, they are much less selective about their targets than the other two types (T-and B-cells).
 |
| Immune Response |
Cell Mediated Immunity:
T-Lymphocytes that have been activated in the thymus gland are released into the circulation. When they encounter their antigen for the first time, they become sensitised to it. If the antigen has come from outside the body,it needs to be presented to the T-lymphocyte on a surface of an antigen presenting cell, including macrophages.These are the part of the non-specific defences, because they engulf and digest antigens indiscriminately, but they also participate in immune responses. To do this, after digesting the antigen they transport the most antigenic fragment to their own cell membrane and display it on their surface. On Their journey around the body, still displaying the antigen fragment, they eventually come into contact with T-lymphocyte that has been processed and target that particular antigen.
 |
| Cell and Antibody Mediated Immune Response in Tabular Form |
If the antigen is an abnormal body cell, such as a cancer cell, it too will be displaying foreign (non-self) material on its cell membrane that will stimulate the T-Lymphocyte. Whichever way the antigen is presented to the T-Lymphocyte are produced, each of which is still directed against the original antigen, but which will tackle it in different ways.
Memory T-Cell:
These long-lived cells survive after the threat has been neutralised, and provide cell-mediated-immunity any responding rapidly to another encounter with the same antigen.
Cytotoxic T-cell:
These directly inactive any cells carrying antigens.They attached themselves to the target cell and release powerful toxins, which are very effective because the two cells are so close together.The main role cytotoxic T-lymphocyted is in destruction f abnormal body cells, e.g/ infected cells and cancer cells.
Helper T-cells:
These are essential fr correct functioning of not only cell-mediated immunity. Their central role in immunity is emphasised in situations where they are destroyed, as by the Human Immunodeficiency Virus (HIV). When helper T-lymphocyte numbers fall significantly, the whole immune system is compromised. T-helpers are the commonest f the T-lymphocytes; their main functions include:
1) Production of special chemicals called cytokines like Interleukins and interferon which support and promote cytotoxic T-lymphocytes and macrophages.
2) Cooperating with B-lymphocytes to produce antibodies ; although B-lymphocytes are responsible fr antibody manufacture, they require to be stimulated by a helper T-Lymphocyte first.
Supressor T-Cells:
These cells act as "brakes" turning off activated T and B lymphocytes. This limits the powerful and potentially damaging effects of the immune response.
 |
| Cell and Antibody Mediated Immune Response in Tabular Form |
ANTIBODY-MEDIATED (HUMORAL) IMMUNITY:
B-lymphocytes, unlike T-lymphocytes, which are free to circulate around the body, are fixed in lymphoid tissue.B-lymphocytes, unlike T-lymphocytes, recognise and bind antigen particles without having to be presented with them by an antigen presenting cell. Once its antigen has been detected and bound, and with the help of a helper T-lymphocyte, B-lymphocyte enlarges and begins to divide.It produces two functionally distinct types of cell, plasma cells and memory B-cells.
 |
| Picture of Antibody mediated immune response |
Plasma cells:
These secretes antibody antibodies into the blood. Antibodies are carried throughout the tissues,while the B-lymphocytes themselves remain fixed in lymphoid tissue.Plasma cells live no longer than a day, and produce only one type of antibody,which targets the specific antigen that originally bound to the B-lymphocyte. Antibodies: Bind to antigens, labelling them as targets for other defence cells such as cytotoxic T-lymphocytes and macrophages.Bind to bacterial toxins,neutrilising them.
Activate complement.
Memory B-cells:
Like memory T-cells, these cells remain in the body long after the initial episode has been dealt with and rapidly respond to another encounter with the same antigen by stimulating the production of antibody-secreting plasma cells.
The interdependence of the body does not normally develop immunity to its own cells is due to the fine balance that exists between the immune reaction and its suppression. Autoimmune diseases are due to the disturbance of this balance.
 |
| 3D picture of Antibody |
 |
| Different parts of Antibody and its spectroscopic picture of Antibody |
ACQUIRED IMMUNITY:
When antigens, e.g. microbes, are encountered for the first time, a primary response follows, in which a low level of antibodies can be detected in the blood after about 2 weeks. Although the response may be sufficient to deal with the antigen, the antibody levels then fall unless there is another encounter with the same antigen within a short period of time.The second encounter produces a secondery response characterised by a rapid memory B-cell response, rsulting ina marked increase in antibody production. Further increases can be achieved by later encounters but eventually a maximum is reached. This principle is used in active immunisation aganist infectious diseases.
Immunity may be acquired naturally or artificially and both forms may be active or passive. Active immunity means that the individual has responded to an antigen and produced his own antibodies, lymphocytes are activated and the memory cells formed provide long lasting resistance.In passive immunity the individual is given antibodies produced someone else. The antibodies eventually break down, so passive immunity is relatively brief.
 |
| Different Types of Acqauired Immunity |
Active naturally acquired immunity:
1) Having the diseases:
During the course of the illness, B-lymphocytes develop into plasma cells that produce antibodies in sufficient quantities to overcome the infection,After recovery, the memory B-cells retain the ability to produce more plasma cells that produced the specific antibodies, conferring immunity to future infection by the same microbe or strain of microbe.
2) Having a subclinical infection:Sometimes the microbial infection is not sufficiently severe to cause clinical disease but stimulates sufficient memory B-cells to establish immunity.
 |
| Medicine and Vaccines help to acquire active artificial immunity |
Active artificially acquired immunity:
This type of immunity develops in reponse to the administration of dead or live artificially weakened microbes(vaccines)or deactivated toxins (toxoid). The vaccines and toxoid retain the antigenic properties that stimulate the development of immunity but they cannot cause the disease. Many infectious diseases can be prevented by artificial immunisation.
 |
| Hospital treatment of diseases |
Passive naturally acquired immunity:
This type of immunity is acquired before birth by the passage of maternal antibodies across the placenta to the fetus, and to the baby in breast milk.
 |
Passive naturally acquired immunity:
This type of immunity is
acquired before birth by the passage of maternal antibodies across the
placenta to the fetus, and to the baby in breast milk. |
Passive artificially acquired immunity:
In this type ready made antibodies, in human and animal serum are injected into the recipient. The source of the antibodies may be an individual who recovered from the infection, or animals commonly horses, that have been artificially actively immunised.
 |
| PRINCIPAL SUBSTANCES RELEASED IN INFLAMMATION and its reaction |
PRINCIPAL SUBSTANCES RELEASED IN INFLAMMATION:
1) HISTAMINE:
Mast cells (in most tissue)
Besophils (Blood)
Stored in cytoplasmic granules. Vasodilation,itching.
2) SEROTONIN:
Platelets.
Mast cell and basophils.Vasoconstriction.
3) PROSTAGLANDINS:
Nearly all cells. Fever, pain
4) HEPARIN:
Liver Mast cells, Basophils. Anticoagulant
5)BRADYKININ:
Tissue and blood.When blood clots, in trauma and inflammation.




























































.jpg)












 Online Movies
Online Movies